A lack of investment in community services and its nursing workforce has left the NHS in a ‘critical condition’, a major investigation into the state of the health service has found.
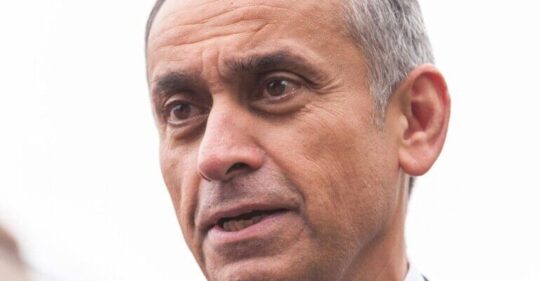
Cancer surgeon and former Labour minister Lord Ara Darzi has published the findings of his highly anticipated review – which was called for by the government and will feed into a new 10-year plan to ‘radically reform’ the NHS.
Lord Darzi placed a stark lens on the impact of a community nursing workforce that has failed to grow in line with increased demand.
He recognised that for almost two decades successive governments have promised to shift care away from hospitals and into the community, and called for ‘financial flows’ into community and primary care services to be hardwired and locked in to ensure this shift could now happen once and for all.
‘Too many people end up in hospital, because too little is spent in the community,’ the review, which draws on evidence from national bodies, NHS staff and government analyses, said.
A&E departments have become ‘congested’ because the government has ‘underinvested in the community’, it added.
While noting that workforce data was hard to pin down, Lord Darzi said he believed the UK has ‘far fewer’ nurses working outside of hospitals compared to other countries and that the UK has ‘too few resources in the community’.
Between 2009 and 2023, the number of hospital nurses working with adults increased by 35%, while those working in children’s hospitals was up 75%, the report said.
Related Article: Dr Crystal Oldman reflects on decade as head of ‘trailblazing’ QICN
In contrast, the number of nurses working in community settings has fallen by 5% over the same period.
And concerningly, the number of health visitors has declined by almost 20% between 2019 and 2023, the report noted.
Analysis suggests the UK could be as much as 86.7% below the Organisation for Economic Co-operation and Development (OECD) average in the number of nurses and midwives working outside hospitals, the report said.
‘Since at least 2006, and arguably for much longer, successive governments have promised to shift care away from hospitals and into the community,’ Lord Darzi said.
‘In practice, the reverse has happened. Both hospital expenditure and hospital staffing numbers have grown faster than the other parts of the NHS, while numbers in some of the key out-of-hospital components have declined.’
The report added that between 2006 and 2022, the share of the NHS budget spent on hospitals increased from 47% to 58%.
Spending in primary and community settings has ‘a superior return on investment when compared with acute hospital services’, Lord Darzi said in his report, adding that it ‘therefore makes sense that this should be the fundamental strategic shift that the NHS aspires to make’.
Overarchingly, Lord Darzi warned the NHS was in a ‘critical condition’ but he stressed its ‘vital signs are strong’.
In the last 15 years, Lord Darzi believes the NHS has been hit by three ‘shocks’, including ‘austerity and starvation of investment, confusion caused by top-down reorganisation, and then the pandemic’.
His report concluded that the health service was continuing to ‘struggle with the aftershocks of the pandemic’ and that is ‘managerial capacity and capability have been degraded’.
The ‘trust and goodwill’ of many frontline staff has also ‘been lost’, he added.
Related Article: Improving clinical competencies and communications in social care in the South East
‘The service has been chronically weakened by a lack of capital investment which has lagged other similar countries by tens of billions of pounds,’ the report said.
‘All of this has occurred while the demands placed upon the health service have grown as the nation’s health has deteriorated.’
Despite this, Lord Darzi believes the NHS can be saved and repaired and set out some ‘important themes’ on how to do this.
These included:
- Re-engage staff and re-empower patients
- Lock in the shift of care closer to home by hardwiring financial flows
- Simplify and innovate care delivery for a neighbourhood NHS
- Drive productivity in hospitals
- Tilt towards technology
- Contribute to the nation’s prosperity
- Reform to make the NHS structure deliver
Responding to the report, health and social care secretary Wes Streeting said the findings would ‘inform our 10-year plan to radically reform the NHS and get patients treated on time again’.
‘The damage done to the NHS has been more than a decade in the making. We clearly have a long road ahead,’ he added.
‘But while the NHS is broken, it’s not beaten. We will turn the NHS around so it is there for you when you need it, once again.’
Royal College of Nursing (RCN) general secretary and chief executive, Professor Nicola Ranger, said: ‘Nursing staff will recognise many of Lord Darzi’s conclusions, not least how sustained austerity, cuts to public health and failure to invest in community services have impacted NHS performance and patient care.
Related Article: Care leaders demand government action to achieve fair pay agreement
‘Moving care into the community and supporting people to live healthier lives is key to repairing our health service, taking that pressure and congestion off the hospital and even more importantly improving population health.
‘But a fundamental shift to a community care model cannot simply be wished into existence, especially with thousands fewer specialist community nurses.
‘Only dedicated investment to boost recruitment into nursing can ensure we have enough highly trained staff, where patients need them.’
On Wednesday, the RCN revealed new analysis suggesting the specialist nurse workforce – including district nurses, health visitors and school nurses – was on track to halve in size over a 20-year period.